Pain
an unpleasant sensory and emotional experience
Even years after my serious illness, I suffer from different pains which influence my life in many different ways. I’ve searched for ways to understand what pain is and what meaning it has in my life.
The topic “pain” was something which I found very interesting and so it was ever-present. Again and again I read articles, books, or researched online, in order to increase my own knowledge and experience. My goal was and is to understand pain so that I am better able to stand it.
The topic of acute or chronic pain has been confronting me since my own illness but also almost daily with ill people in my position as Chairwoman of the charitable organization TEB e.V. Selbsthilfe (Self-help group) and as supervisor of the various regional self-help groups.
Pain is a part of our lives
Affected persons talk to me about their experiences with pain and their feelings in many conversations and consultations. In the process of these conversations, I noticed that each person perceives his/her pain and his/her sense of pain differently. Pain has many faces and facets.
In medicine pain is described as an unpleasant sensory experience which is linked to real and potential tissue damage.
And still pain is important and effective and part of our life, exactly because it gives us this unpleasant feeling. Pain has a very important warning function and the job of protecting our bodies from damaging and dangerous influences.
In everyday life pain is unpleasant and is often a bad sign. On the one hand that’s correct, on the other hand pain protects and saves us, and warns us of danger and does that before injury occurs or we injure ourselves further.
Pain often forces us to perhaps move, think or behave differently. Pain is an important signal and often saves us from worse.
There can be different reasons for pain being triggered, e.g. cold or heat; inner disorders and troubles with the nervous system. There are nerve fibres almost all over the body with quite different receptors, which transfer the different stimuli to the brain. Our brain has no pain receptors of its own and therefore doesn’t feel pain.
At the same time the pain system in our bodies can act in a way that we find strange. For example, the pain in an infected finger is sometimes not noticed until it is hot and swollen or if it’s stiff. Usually you notice the pain more quickly and more intensively, if there’s blood as well.
But there is not always pain. Sometimes the pain system fails, for instance in the case of pancreatic cancer. Affected persons report that they never had pain or other problems with the pancreas. When their strong pain then started up, it was too late for a cure.
We believe that experience with pain is normal and that our body signals each unpleasant reaction. But that is not always the case. Very often pain which is present e.g. in joints, muscles, nerves and in the immune system is not noticed by the body because our brain does not see them as a threat.
It’s also possible that phantom pain is felt because the brain recognizes a threat or because it is anchored in our pain memory already, although the body part where the pain is felt is missing (amputated).
Sorrow, grief, affliction and loneliness are sometimes felt as physical as well as psychological pain. It is often said that the soul is screaming and the body reacts to that.
If we include psychological pain as well as physical pain, then it becomes clear to everyone that we have to examine pain from all directions.
Pain is always a very individual, personal sensation and often has no physical origin.
Chronic pain is an independent illness which lost its warning function. Psychological pressure can lead to physical pain. Joy can reduce the pain, sorrow can increase it. Thoughts, feelings and perceptions play a large role in all pain experiences and sensations.
Pain originates when mechanical (e.g. car accidents), thermic (e.g. scalding), chemical and electrical stimuli cross a certain threshold in the body. The damaged tissue reacts and releases signal substances which bind themselves to special pain receptors (nociceptors). These are free nerve ends, which are specialized on the perception and transmission of painful alterations. We have nociceptors in skin, muscles, bones, joints and inner organs, which report an incoming pain to the spinal cord.
What are the functions of the spinal cord and brain?
The pain impulse is transported from the spinal column through the nerves up to the brain. Our nerve lines intersect in the spinal cord, i.e. if a pain occurs on the left-hand side of the body, then it is transferred to the right-hand side of the brain or the other way around. The incoming information is processed in the brain. Where is the pain? How bad is it? The brain assesses the pain and its perception by linking to the limbic system which, for example, is responsible for the creation of feelings. That’s the reason why pain is often felt to be very unpleasant and irritating.
The body reacts to pain!
When a pain signal reaches our brain the body starts a defensive reaction against the origin of it almost immediately. The body’s own pain-reducing system is started in the brain if the body is unable to react due to, for instance, a severe accident. The hypothalamus stimulates the flow of Noradrenalin, which causes the heart beat to change its speed, the blood pressure to rise and increases transpiration.
The body’s own inhibitors, called endorphins, can definitely help to reduce pain or even deactivate it altogether. They prevent the transmission of pain signals and that way change the way we feel the pain. These inhibitors only work for a short time and are released during physical exertion or under the threat of danger. That’s the reason why we only feel the pain when our body relaxes or the danger has passed.
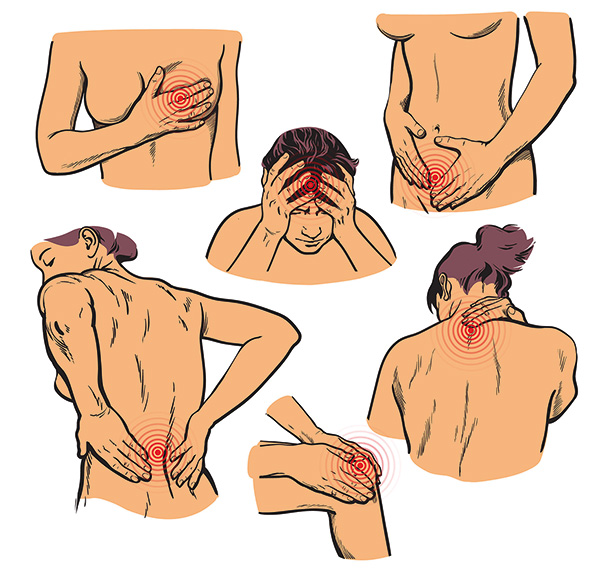
What kinds of pain are there?
- Sudden unexpected pain (colic)
- Throbbing, burning pain (burns)
- Deep, piercing pain (slipped disc)
- Dull pain (headache)
Pains can be classified according to how they originate and what they feel like. These different categories are important, as pain reacts in different ways to pain killers. Depending on what causes the pain, one speaks of:
Nociceptor pain
This pain is caused by external influences like e.g. blows, scalding and burning, bruising or by inflammation, tumours, colic, and blockages. In the case of abdominal colic the muscles of the abdominal organs contract more strongly, which immediately stimulates the pain receptors. Inflammatory illnesses like rheumatism, toothache and earache are also among the nociceptor pains. In neuropathic pain the peripheral and central nerve fibres are damaged. The pain does not report tissue damage, but its own dysfunction. Typical for neuropathic pain are severe, often razor-sharp or burning pains. They occur briefly and suddenly, but the affected person perceives them as long, dull and continuous. Polyneuropathy, slipped discs and phantom pain are some examples.
Reflectory pain
This pain can result from incorrect regulation or bad posture e.g. migraines, tension headaches, backache or an illness in which injuries cause a complex disease of the connective nerve tissue.
Psychosomatic pain
The pain can also result from psychological stress and for example cause headache. At the same time, pain is a great psychological burden and therefore the cause or effect of the pain can hardly be determined. Who screamed first, the body or the soul?
Visceral pain
is a pain that comes from the internal organs. It is usually dull and difficult to isolate. The corresponding areas on the body surface are also called Head's zones. Their position is usually the same as that of the affected organ. In some cases, the Head's zone and the actual origin of the pain are far apart. For this reason, sufferers often experience long periods of back pain before the diagnosis of pancreatic cancer is made.
Somatic pain
This pain can be divided into two different areas: deep or surface pain. Deep pain comes from bones, muscles, joints and connective tissue. It is dull, often radiant and is accompanied by vegetative symptoms e.g. nausea, trembling, perspiration. On the other hand surface pain originates in the skin or mucous membranes and are usually caused by irritations of the skin and can be ascribed to an inflammation or injury. They’re easy to locate, fade away quickly, once the triggering impulse has been found and treated. Affected persons in the different groups and in various conversations describe exactly this sort of pain. The people report that they have developed a different sense of pain. They suspect that their sense of pain has changed to make them more sensitive.
As one affected person said: “I cannot bear any pain for long now since pancreatic cancer was diagnosed, I need painkillers much more quickly and more often and usually also need a higher dose. I have the feeling that I have become more sensitive to pain over time. Nowadays I feel pain before anything is done to me.”
“It’s the same for me. I have also become more sensitive to pain. I’m sure that, in my case, fear plays a large part, it makes the pain feel worse. So, now I feel the pain before, for instance, I get a needle inserted for a blood sample, because I was always scared of needles and injections.”
“Yes, it’s the same for me,” says another affected person and the next one says: “It’s similar for me.” They continue talking and say: “I think that it’s due to the fact that we are familiar with the therapies and treatments we have to endure, that we know what is going to happen and are scared and this fear expresses itself as pain. I always experience this with the aftercare appointment. I get cramps and colicky pains, together with diarrhea and as soon as the consultation is over I feel better. “
The personal attitude towards taking medication is not nesessarily correct
Affected persons have a very individual way of approaching and dealing with their pain. Many want to be strong and bear the pain. They want to do without painkillers or take them the way they think is right for them because they’re scared that they might possibly become addicted, depressed, tired, feeble and exhausted. They are convinced that they are doing the right thing if they take painkillers when they can no longer bear the pain.
An attitude like that can have negative consequences because painkillers should be taken precisely according to prescription. Morphine, for example, should be taken so that the patient has a constant level in his/her body and an additional medicament can be given in case of pain peaks.
I notice again and again in conversations with affected persons and their relatives that there are very different pains and different ways of coping with them.
Once, in one of my consultations with an affected person, I had someone who was dreadfully afraid of chemotherapy, because he had experienced how his mother had suffered. His fear was so great that, when I only mentioned the word chemotherapy, he suffered considerable abdominal pain and rushed off to the toilet.
One could hardly do anything here with reason, good words or explanations, his pain and his attitude to chemo did not allow that one could administered and he accepted the risk that he might lose valuable time and therefore also an opportunity.
Unfortunately, doctors have less and less time for their patients
His doctor noted his fear but didn’t have the time to find out the cause of his fear and why the affected person suffered from violent abdominal pain as soon as he heard the word chemo.
On the other hand, self-help means first of all time and listening. I wanted to understand what the background was, because, only if I understand, can I perhaps find ways of reaching the affected person and can help him to review his situation again.
In the first conversation with the affected person I could easily feel his enormous fear. He was scared that he would have to endure and suffer the same as his mother had to do. He could hardly think clearly, he just kept repeating that he didn’t want to have to suffer the same as his mother.
Sometimes many conversations are necessary
I had many talks with him and was able to convince him that his mother’s illness was indeed dreadful and sad, but that it was her illness, her ordeal and her fate. I was also able to explain that a modern chemo-therapy is different and that the side effects can be treated differently. We arranged a meeting together with his doctor and he explained to us why he thought a chemo was a good idea.
After that we made an agreement for him to have 2 chemo treatments. It was agreed that if he felt that it was impossible to continue, we would stop without any discussion. Again, we also agreed that he might phone me anytime, if he had the feeling that I would be able to help him.
So, what can I say? All the chemo’s which he got up to now, went off without a hitch and also the side effects were minimal and were easily treated.
A few weeks ago he came to me in the office to thank me. He said that he had lost his fear and also the pain. He thanked me for taking the time to understand my fear and the pain resulting from it.
We talked for a long time and I asked him if his doctor wouldn’t have been able to disabuse him of his fear. Indeed, it turned out that his doctor intended trying the same way I had done, but the affected person closed up. He didn’t believe the doctor because he thought that he wanted to earn something in the first place and would therefore not be neutral.
I could report on lots of situations and pains that our group members at TEB e. V. have and where I experience that pain is caused by fear and is very troublesome for the people.
Fear can protect and lame simultaneously
Recurring pain must be treated, because otherwise it can become trapped in the pain memory, be saved there and then signal pain where there is none.
No-one wants any pain and if pain occurs then it should be treated swiftly so that it can disappear again very quickly. Continuous pain, which isn’t treated quickly enough can lead to the thought of killing oneself, one affected person reported.
Nowadays it is seldom necessary to often have to suffer strong pain, there are different medicines and therapies, which help us, to live a normal and bearable life in spite of the pain.
Katharina Stang
Speak to your doctor, talk openly about your pain and your feelings. If you require to, take the correct medicine that your doctor has prescribed, in sufficient quantities and in good time. Don’t act on your own authority.
Katharina Stang
Source:
https://www.internisten-im-netz.de/krankheiten/schmerzen/schmerzformen.html