Pancreatic Cancer
Pancreatic cancer develops from the exocrine glands (the glands which flow out of the pancreas). In addition to that there are endocrine tumours (developing in the endocrine or ductless glands) and other tumours e.g. IPMN: intraductal-papillary-mucinous neoplasm.
10 of 100000 inhabitants are affected yearly. This form of cancer is one of the worst types and is at the top of the list of causes of death. The illness usually occurs in elderly people.
The cause of this illness is largely unknown, however there’s a hereditary risk in some of the cases. Risk factors which can favour the outbreak of cancer are: old age, gender (men are more often affected), hereditary factors, chronic pancreatitis, alcohol, nicotine misuse, and dangerous substances like nitrosamines.
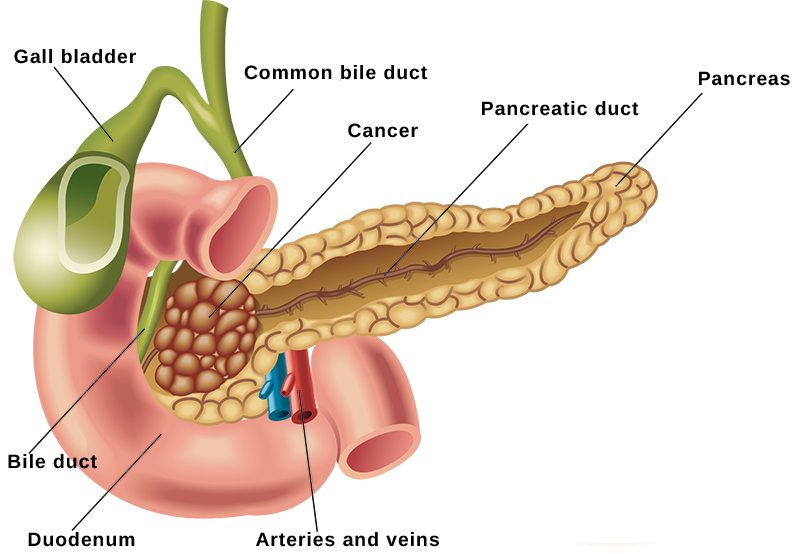
In 60% of the cases pancreatic cancer strikes the head of the pancreas and then in the remaining cases the middle part and the tail area.
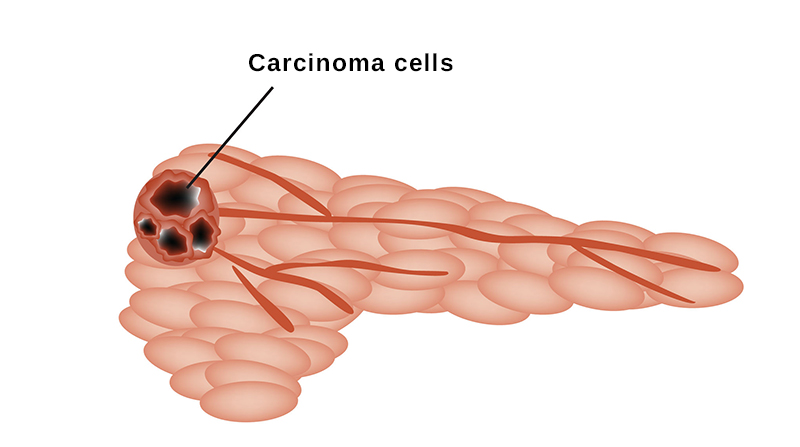
Most of the tumours are adenocarcinoma, which develop out of the glands of the pancreas. Unfortunately, the tumour expands into neighbouring tissue and further structures in an early stadium. The cancer presses on the bile-duct and the digestive enzyme duct fairly early on in its development. Affected persons therefore often suffer from icterus very early on in the illness. Pancreatic cancer metastasises rapidly in the neighbouring organs: liver, peritoneum, spleen, lungs and bones. The first indications of an illness can be: pains in a ring-like fashion in the upper abdomen, back pain, problems of the digestive tract like diarrhoea, nausea, vomiting, loss of appetite, slow weight loss and a possible jaundice. The stools change as well, becoming lighter, thinner, mushy and strongly-smelling.
These are all the signs of a fatty stool. Urine often gets darker. The symptoms of jaundice and digestive problems often occur when the tumour is in the pancreas head, while pancreoprivic diabetes 3c and thrombosis of the spleen can occur when the tumour is in the middle or tail area.
Pancreatic cancer is often only diagnosed when it is too late, because the symptoms tend to be of a general kind. The following examinations are helpful in diagnosing: ultrasound, endosonography, computed tomography (CT) and magnetic resonance tomography (MRT) and ERCP (endoscopic retrograde cholangiopancreatography). Should it be necessary, then a tissue biopsy will help to clarify the situation.The only possible chance of healing is an early operation (Whipple, Traverso etc.) Unfortunately, only around 20% of patients benefit from this possibility. Admittedly, those who are not able to be operated on can live for quite a long time thanks to good treatment (chemotherapy, diet, pain therapy etc.) For some years now it has been possible to reduce the size of the tumour using neoadjuvant chemotherapy to make it operable.
At the moment a good chemotherapy can be administered using gemcitabine, 5-FU, folfirinox and the combination of gemcitabine and nabpaclitaxell together. Naturally, other combinations can be considered individually for each patient. Currently, new immunotherapies with immune checkpoint inhibitors are being examined, e.g. nivosumab, hyperthermia, IRE (irreversible Electroporation) and others. As far as complementary medical procedures are concerned there are the following possibilities: mistletoe therapy, l-Carnitine, Sulforaphane and others.
The complementary medicine treatments are contested by allopathic practitioners while the holistic practitioners advocate them.
Joachim Horcher