Acute Pancreatitis
Pancreatitis (= Inflammation of the Pancreas) generally takes one of the two forms: acute or chronic
We will be discussing the acute form in this article.
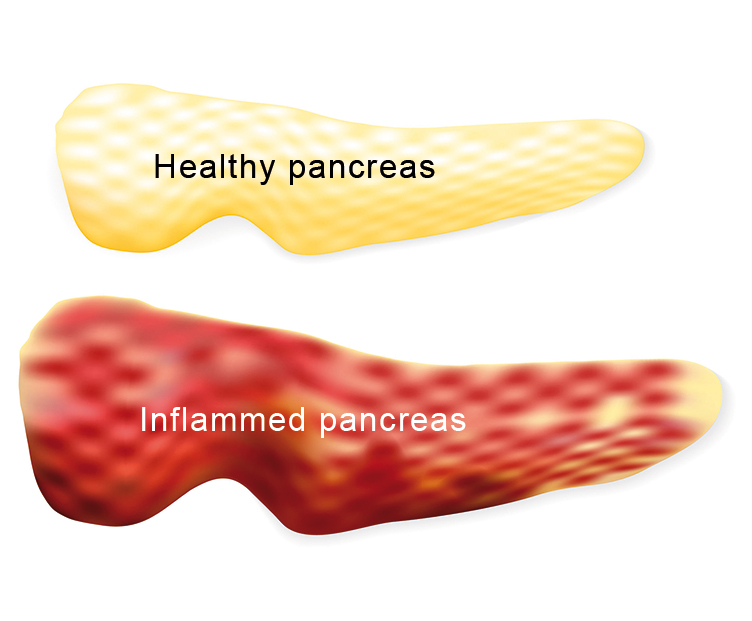
Acute Pancreatitis is the sudden inflammation of the pancreas. Principal causes are stones in the gall bladder, which can block the channels in the pancreas, and alcohol misuse. Further causes can be side-effects of medicines (e.g. ACE-inhibitors, glucocorticoids), hereditary factors, metabolic disorders, infectious illnesses, inborn malformations of the pancreas, tumours, abdominal injuries, autoimmune disorders etc. Clinical examinations (e.g. ERCP) can also trigger a pancreatitis. Affected persons often experience strong or even very strong pain in the upper and middle abdomen, which can radiate in a ring-like form out to the sides and around the back. In addition to that, nausea, vomiting, flatulence and a temperature can also occur. The pain sometimes moves up into the chest and resembles a heart attack. Further symptoms that are possible: bowel paralysis or blockage (ileus), circulatory disorders and a huge accumulation of fluid in the abdominal and in the thoracic cavity. The affected persons are seriously ill.
The diagnosis can be determined through clinical examinations, laboratory tests and body-imaging. The laboratory results show a massive rise in the lipase and alpha-amylase. If the illness is caused by gall stones then additional tests (gamma GT, AP=alkaline phosphatase and Bilirubin) will be necessary.
The clinical examination shows that the abdomen is of a plump but elastic consistency, and, in the case of gall stones as the cause, jaundice, (darker urine, skin and the conjunctivas are yellow). The main body-imaging examination in this specific case is ultra-sound followed by CT (computed tomography) and MRT (nuclear magnet resonance imaging).
Severity and the courses it can take
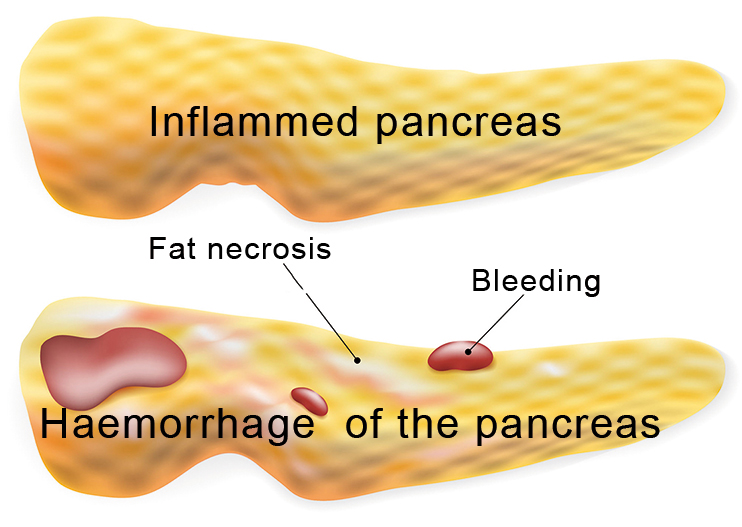
Acute pancreatitis can occur in different forms and levels of severity. In the milder cases (acute oedematous pancreatitis, approx. 85% of all cases) the pancreas swells through the inflammation, but usually heals again without any complications. In the more severe cases (necrotizing pancreatitis, approx. 15% of all cases) with partial or complete necrosis (death of cells or tissue) of the pancreas then the prognosis is much worse, especially because further organs (lung, heart, colon, kidneys) could be affected, which can be life-threatening in the end. The destruction of the pancreatic tissue can lead to a permanent loss of function making enzymes necessary to ensure digestion and possibly an onset of diabetes. The dead tissue can cause considerable problems like pseudo cysts, abscesses, blockages, infections and sepsis, which often make a surgical intervention necessary.
Acute pancreatitis must be treated intensely in hospital. The treatment differs according to the cause of the illness (endoscopic removal of gall stones, abstinence.) It is especially important that infusions are placed immediately to replace the missing body fluid, which can be considerable. Another thing which is indispensable is sufficient painkillers. If it is a mild form of the illness then eating should be resumed soon, while a drip-feed should be installed as soon as possible for the more serious forms. Antibiotics are usually necessary with a necrosis, for an infection of the necrosis centres could lead to sepsis.
Should the illness take a severe course, then additional intensive-care measures such as artificial respiration, correction of the acid-base balance, dialysis and also surgical intervention may be necessary.